ECHS reimbursement claims are often rejected or delayed due to small procedural errors rather than medical issues. Understanding the common rejection reasons and knowing how to avoid them can save Ex-Servicemen and their families significant time, stress, and money.
This guide explains why ECHS claims get rejected and gives practical solutions to ensure smooth approval.
What Is ECHS Reimbursement?
ECHS reimbursement applies when:
- Treatment is taken in a non-empaneled hospital (usually emergency), or
- Payment is made by the beneficiary and later claimed, or
- Certain medicines/tests are not available at ECHS dispensaries.
Reimbursement is processed strictly as per ECHS SOP & CGHS rates.
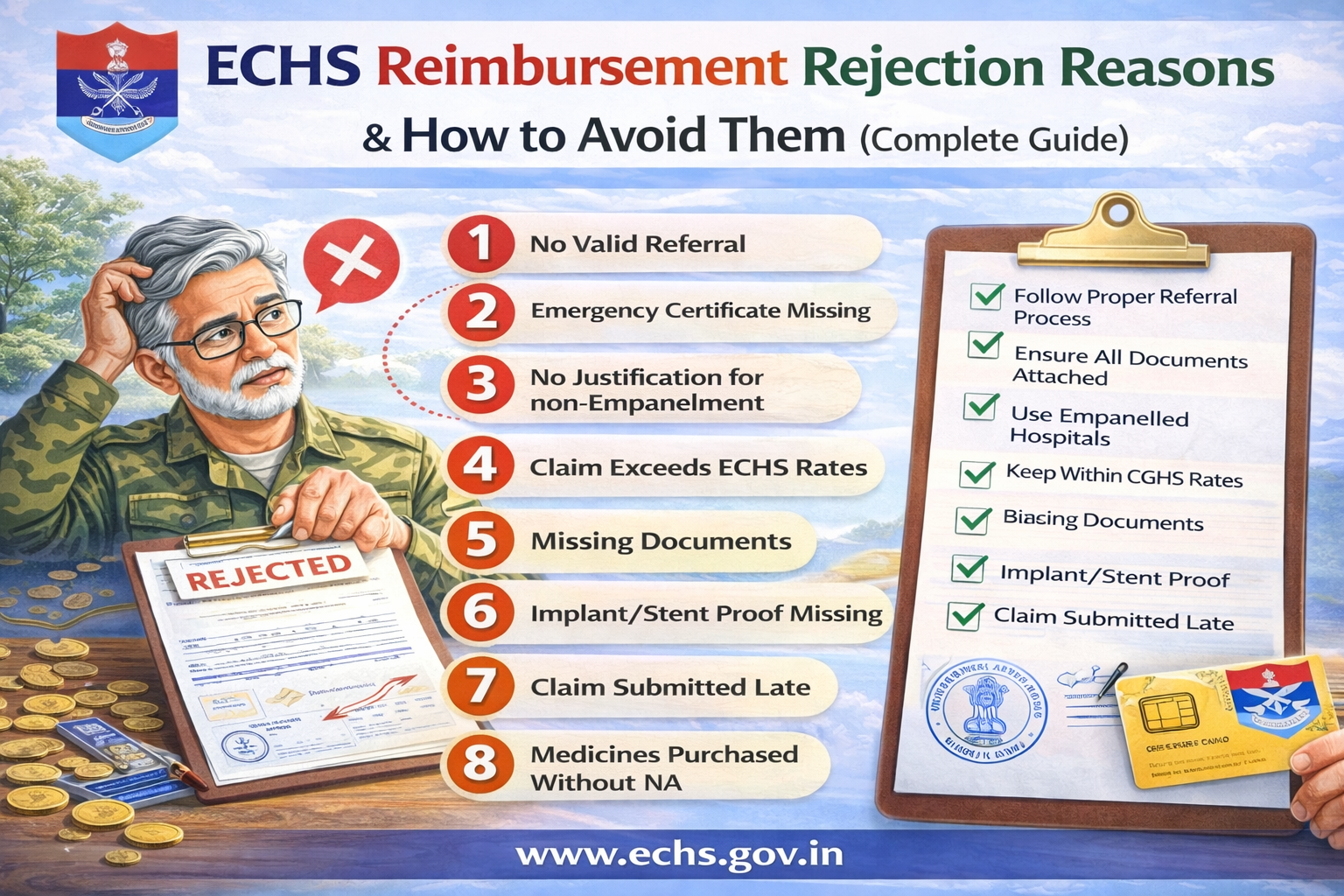
Top Reasons for ECHS Reimbursement Rejection
1. ❌ Treatment Without Valid Referral
Reason
- No ECHS referral letter attached
- Referral expired (valid only for 1 month, except oncology)
How to Avoid
- Always obtain referral from ECHS Polyclinic
- For follow-ups, ensure referral clearly mentions duration
- Keep photocopies of all referrals
2. ❌ Emergency Certificate Missing or Invalid
Reason
- Emergency treatment taken but no emergency certificate
- Certificate not signed/stamped by hospital authority
How to Avoid
- Obtain Emergency Certificate + EIR
- Hospital must inform ECHS within 48 hours
- Emergency must match approved emergency conditions
3. ❌ Treatment in Non-Empanelled Hospital Without Justification
Reason
- Empanelled hospital available but not used
- No proof of non-availability
How to Avoid
- Use empanelled hospital whenever possible
- Attach NA (Non-Availability) Certificate if applicable
4. ❌ Claim Exceeds CGHS/ECHS Rates
Reason
- Hospital charges higher than approved rates
- Private ward used without entitlement
How to Avoid
- Check ward entitlement based on rank
- Reimbursement limited to CGHS rates, even if paid more
5. ❌ Missing or Incomplete Documents
Reason
- Missing discharge summary
- Bills not itemized
- Reports not signed or stamped
How to Avoid
Attach all mandatory documents:
- Referral letter
- Discharge summary
- Itemized bill + final bill
- Investigation reports
- Implant invoices & stickers (if applicable)
6. ❌ Implant / Stent Proof Not Attached
Reason
- Implant pouch/sticker missing
- Invoice does not mention patient name or batch number
How to Avoid
- Always collect:
- Implant outer pouch
- Batch number sticker
- Original invoice
Without these, implant cost is rejected fully.
7. ❌ Delay in Submission of Claim
Reason
- Claims submitted after 1 month from discharge
- No delay waiver approval
How to Avoid
- Submit claim immediately
- Delay up to 6 months → Station Commander approval
- Beyond 1 year → Central Organisation decision
8. ❌ Medicines Purchased Without NA Certificate
Reason
- Medicines available in ECHS dispensary
- No NA certificate from polyclinic
How to Avoid
- Collect NA certificate before purchasing medicines
- Only specific cases allow medicine reimbursement
9. ❌ OPD Claims Without Proper Proof
Reason
- OPD slip missing
- Doctor’s signature absent
How to Avoid
- Attach:
- Referral letter
- OPD consultation slip
- Doctor’s signature & stamp
10. ❌ Package Procedure Billed Incorrectly
Reason
- Extra charges billed during package period
- Diet, nursing, ICU billed separately
How to Avoid
- Package includes:
- Room rent
- Medicines
- Nursing
- Investigations
- Extra billing allowed only beyond package duration with approval
How to Ensure 100% Claim Approval
✅ Before Treatment
- Verify empanelled hospital
- Confirm ward entitlement
- Collect referral or emergency certificate
✅ During Hospitalization
- Keep all reports
- Ask hospital for ECHS-compliant billing
✅ After Discharge
- Arrange documents chronologically
- Number each page
- Submit both online (UTIITSL) and physical copy
What to Do If Your ECHS Claim Is Rejected?
- Ask polyclinic for written rejection reason
- Rectify documents (if curable)
- Resubmit claim
- If unjustified, appeal through Regional Centre → Central Organisation
Claims cannot be rejected at intermediate levels without forwarding.
Frequently Asked Questions (FAQs)
❓ Can ECHS reject a claim completely?
Yes, if:
- No emergency
- Fraudulent claim
- Non-compliance with SOP
❓ Is ambulance reimbursement allowed?
❌ No. Ambulance charges are not admissible.
❓ Can I claim from insurance and ECHS both?
Yes, but ECHS reimburses only the balance after insurance.
❓ How long does reimbursement take?
- Normal cases: 30–60 days
- High-value cases (>5 lakhs): longer due to MoD approval
Final Advice for ECHS Beneficiaries
Most ECHS claim rejections are avoidable.
Proper referral, correct documentation, and timely submission are the keys to hassle-free reimbursement.